Laparoscopic Sleeve gastrectomy for weight loss
- Laparoscopic sleeve gastrectomy is a procedure growing in popularity and use to aid weight loss. It combines a low complication rate with effective weight loss.
- Here, we explain some of the aims, benefits, risks and alternatives to this procedure. We want you to be informed about your choices to help you to be fully involved in making any decisions.
- Please ask about anything you do not fully understand or wish to have explained in more detail.
About Laparoscopic Sleeve Gastrectomy
Laparoscopic sleeve gastrectomy involves removing most (75-80%) of the stomach, leaving a narrow gastric ‘tube’ or ‘sleeve’. This limits food intake by reducing the size of your stomach. It causes changes in gut hormones which suppresses your appetite and improves blood sugar control. It does not reduce the absorption of nutrients.
Most patients undergoing sleeve gastrectomy would expect to lose approximately 60% of their excess weight over 18-24 months from surgery.
Laparoscopic or “key hole” surgery, involves placing several small (1-2 cm) cuts on the abdomen rather than a single larger incision. One incision is slightly larger (ie 3-4 cm) to extract the part of stomach being removed from the abdominal cavity. There is always a small chance (1-2%) that laparoscopic surgery may need to be converted to an open operation when a longer incision is made on the abdominal wall.
The diagram below may help you better understand what is done in a laparoscopic sleeve gastrectomy.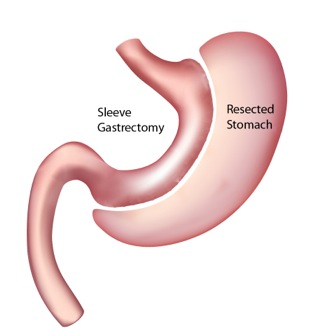
Alternative procedures that are available
- Laparoscopic adjustable gastric banding - involves placing an adjustable plastic band around the upper stomach. In appropriate cases it can achieve good weight loss. However it does require multiple adjustments in the post operative period. It has a risk of needing further surgical intervention in the case of slippage and rarely erosion into the stomach.
- Laparoscopic Bypass (“Roux en Y”) - involves making the stomach into a small pouch connected to the intestine and bypassing a length of intestine. It has effects on appetite and gut hormones like lap sleeve gastrectomy and also causes malabsorption of nutrients. It is a more complex procedure with a slightly higher complication rate.
Before your procedure
- We want to make sure you are fit enough to undergo the operation and it is suitable to help you lose weight.
- You will complete a questionnaire covering important background and be assessed by your consultant and specialist nurse. You will be provided with patient information.
- The next step is assessment by our specialist dietician who will assess you intake and advise fully about preoperative (low calorie ‘liver shrinkage’) diet and about post operative dietary changes.
- Selected patients will be referred for psychological assessment if this is required.
- You will have routine blood tests - sometimes at your GP surgery.
- You will have a preoperative assessment for checking blood pressure and ECG if needed.
- You will usually be admitted to hospital on the day of your operation.
During the procedure
- Before your procedure, you will be given the necessary general anaesthetic.
- The stomach lies within the abdomen and therefore it is necessary to make several small incisions (each 1-2 cm) in your abdomen to allow instruments to be placed adjacent to the stomach. The abdomen is inflated with carbon dioxide to create space to perform the operation and a camera is placed within the abdominal cavity.
- The part of stomach to be removed will then be carefully separated from surrounding tissues and divided from the remaining stomach using a stapling device. It will then be removed. It will be ensured that the site of closure is healthy and watertight.
- You will wake up in the recovery room after your operation. You might have an oxygen mask on your face to help you breathe. You might also wake up feeling sleepy.
- After this procedure, most people will have a small, plastic tube in one of the veins of their arm. This might be attached to a bag of fluid (called a drip), which feeds your body with fluid until you are well enough to eat and drink by yourself.
- While you are in the recovery room, a nurse will check your pulse and blood pressure regularly. When you are well enough to be moved, you will be taken to a ward.
- Sometimes, people feel sick after an operation, especially after a general anaesthetic, and might vomit. If you feel sick, please tell a nurse and you will be offered medicine to make you more comfortable.
- Drain tube: You may have a tube within the abdominal cavity. These are to prevent fluid from accumulating. This will normally be removed after 1 day.
- Getting around and about: Generally, it is best to get out of bed as soon as you feel you can. You will be encouraged to move your legs in bed to prevent blood clots forming.
- When you can leave hospital: People who have had a laparoscopic sleeve gastrectomy will usually stay in hospital for 2 days.
- When you can resume normal activities including work: It is highly variable between different people. You still will have had major surgery, although it will have been performed via a key-hole technique. It will likely take two-four weeks before you are able to return to work – depending on the nature of your work. Heavy lifting should be avoided for six weeks. We will provide you with specific information and instructions on your recovery before you go home.
- Post operative diet: Fluids only for the first two weeks. Then smooth pureed diet for the next two weeks before progressing onto a soft diet. High protein solid textured diet from 2 months. Full details (including written) given during dietetic assessment.
- Supplements: lifelong multivitamin and mineral supplements are recommended. Annual blood checks are advised.
- Pregnancy: it is not advisable to conceive during the period of rapid weight loss in the first 18 months after surgery.
The aim of the surgery is to aid weight loss and reduce to complications that arise from being overweight:
- Type II Diabetes - improved control and resolution in up to 75%
- Hypertension, sleep apnoea, fatty liver, cholesterol level improved in majority.
Serious or frequently occurring risks
- Leak from the stomach – This is an uncommon (approximately 4% risk), but potentially serious complication following laparoscopic gastric surgery. Part of the stomach is removed using special staples. Surgeons take great care and time in ensuring that the closure is secure and watertight. However, in rare cases the closure does not remain water tight. This is often because of a poor blood supply rather than any particular problem with the surgery. If this happens a small amount of stomach contents may leak out into the abdominal cavity. If this does occur, there is a risk of infection and you will require antibiotics and possibly further keyhole surgery or a fine drain tube to be inserted (under local anaesthetic) next to the operation site to get rid of any excess fluid or infection. Most leaks are very small (pin head size) and resolve spontaneously after 5-7 days, without too many problems. In extremely rare cases, patients can become very ill and need to be transferred to the intensive care unit or require more major surgery.
- Chest infection – Surgery carries with it a risk of developing an infection in the lungs or pneumonia and can occur following this procedure (5%). This is usually because you are a little immobile and not breathing deeply following surgery, resulting in the lower part of the lungs becoming stagnant. Chest infections are treated with antibiotics and physiotherapy. It is very important that you get up and moving as soon as possible and work closely with the nursing staff or physiotherapist in making sure you are taking regular, deep breaths. You will be given deep breathing exercises to undertake. The risk of developing a chest infection is greatly increased if you smoke cigarettes (particularly within three months of surgery). Having had the procedure performed using the key hole technique greatly improves your ability to move about following the surgery.
- Complications relating to the heart – Major surgery places considerable stress on the body and there is a small risk of a problem relating to the heart. This may take two forms and varies from very minor to severe. Firstly, the heart may develop an abnormal rhythm (usually beating excessively quickly). You may notice a fluttery feeling (palpitations) in the chest or nothing at all. Usually, simple measures such as balancing the body’s salt concentrations or administering medications resolve these problems. Secondly and more seriously, suffering a heart attack (damage to the heart muscle) is possible. Because of these risks you are very closely monitored for the first few days following your surgery. Therefore, if a problem arises it can usually be treated early and effectively. The risk of developing a heart problem is increased if you have a history of heart problems, smoke cigarettes (particularly within three months of surgery) or have other risk factors for heart disease.
- Death – All surgery carries a risk of death related to the procedure and the anaesthetic. It is estimated that this risk of death with this procedure is less than 1%.
- Deep vein thrombosis (DVT) and pulmonary embolus - All surgery carries varying degrees of risks of thrombosis (clots) in the deep veins of your leg. In the worst case a clot in the leg can break off and travel to the lung (pulmonary embolism). This can significantly impair your breathing. To prevent these problems around the time of your operation and following your operation we give you some special injections to ‘thin’ the blood. We also ask you to wear compression stockings on your legs before and after surgery and also use a special device to massage the calves during the surgery. Moving about as much as you can, including pumping your calf muscles in bed or sitting out of bed as soon as possible reduce the risk of these complications. We normally prescribe blood thinning injections for two weeks after discharge.
- Damage to the bowel (intestines) - Any surgery inside the abdominal cavity is associated with a very small risk (less than 1 in 500 chance) of damaging other organs, such as the bowel. This is particularly the case if there has been previous surgery with scarring and structures are abnormally stuck to each other. If there is damage to the bowel it can almost always be repaired at the time. If it is not noticed at the time and you later become unwell a second procedure may be required. This is a more serious situation.
- Damage to major blood vessels - Any major surgery is associated with a small risk of bleeding from a major blood vessel. This is most uncommon. If this were to occur the surgeon would take measures to stop the bleeding and it is possible you would require a blood transfusion.
- Damage to the spleen - Very rarely, damage to the spleen can occur (<1% risk) that results in bleeding. This is because the spleen is very close to the stomach and is sometimes stuck to the region that needs to be operated on. Most times, bleeding from the spleen is not serious and can be controlled simply, however, if the spleen were to sustain a more severe injury the spleen may have to be removed to prevent further bleeding. Removing the spleen normally has few complications. If your spleen is removed you will be given some vaccinations prior to leaving hospital. Additionally, you will be advised to stay on a low dose of preventative antibiotic for at least two years.
- Bleeding – This very rarely occurs after any type of operation. Your pulse and blood pressure are closely monitored after your operation as this is the best way of detecting this potential problem. If bleeding is thought to be happening, you may require a further operation to stop it. This can usually be done through the same scar(s) as your first operation. It is possible that you also may require a blood transfusion.
- Wound haematoma - Bleeding under the skin can produce a firm swelling of blood clot (haematoma), this may only become apparent several days after the surgery. It is essentially a bruise. This may simply disappear gradually or leak out through the wound without causing any major consequences to you.
- Wound Infection – This affect your scars. If the wound becomes red, hot, swollen and painful or if it starts to discharge smelly fluid then it may be infected. It is normal for the wounds to be a little sore, red and swollen as this is part of the healing process and represents the body’s natural reaction to surgery. It is best to consult your doctor if you are concerned. A wound infection can happen after any type of operation. Simple wound infections are easily treated with a short course of antibiotics.
- Deep Infection – A rarer and more serious problem with infection is where an infection develops inside your tummy or chest cavity. This will often need a scan to diagnose, as there may be no obvious signs on the surface of your body. Fortunately, this type of problem will usually settle with antibiotics. Occasionally, it may be necessary to drain off infected fluid. This is most frequently performed under a local anaesthetic by our colleagues in the X ray department. In the worst case scenario a further operation is required to correct this problem.
- Scarring – Any surgical procedure that involves making a skin incision carries a risk of scar formation. A scar is the body’s way of healing and sealing the cut. It is highly variable between different people. All surgical incisions are closed with the utmost care, usually involving several layers of sutures. The sutures are almost always dissolvable and do not have to be removed. The larger an incision the more prominent it will be. Despite our best intentions, there is no guarantee that any incision (even those only 1-2 cm in length) will not cause a scar that is somewhat unsightly or prominent. Scars are usually most prominent in the first few months following surgery, however, tend to fade in colour and become less noticeable after a year or so.
- Other complications – We have tried to describe the most common and serious complications that may occur following this surgery. It is not possible to detail every possible complication that may occur following any operation. If another complication that you have not been warned about occurs, we will treat it as required and inform you as best we can at the time. If there is anything that is unclear or risks that you are particularly concerned about, please ask.